Trusted Gynecological Expertise
Annual Gynecological Exams
Breast Exams
HPV, Pap Smears, Colposcopy, LEEP, Genital Warts
Gardasil
Contraception
Miscarriage
Ectopic Pregnancy
Abnormal Uterine Bleeding, Endometrial Biopsy
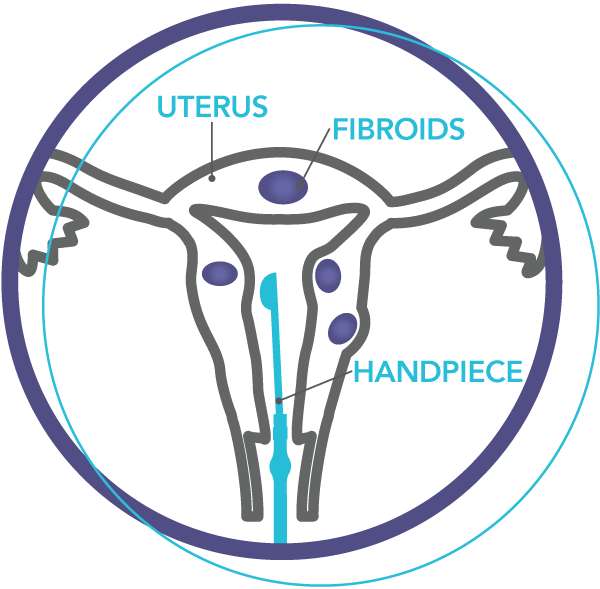
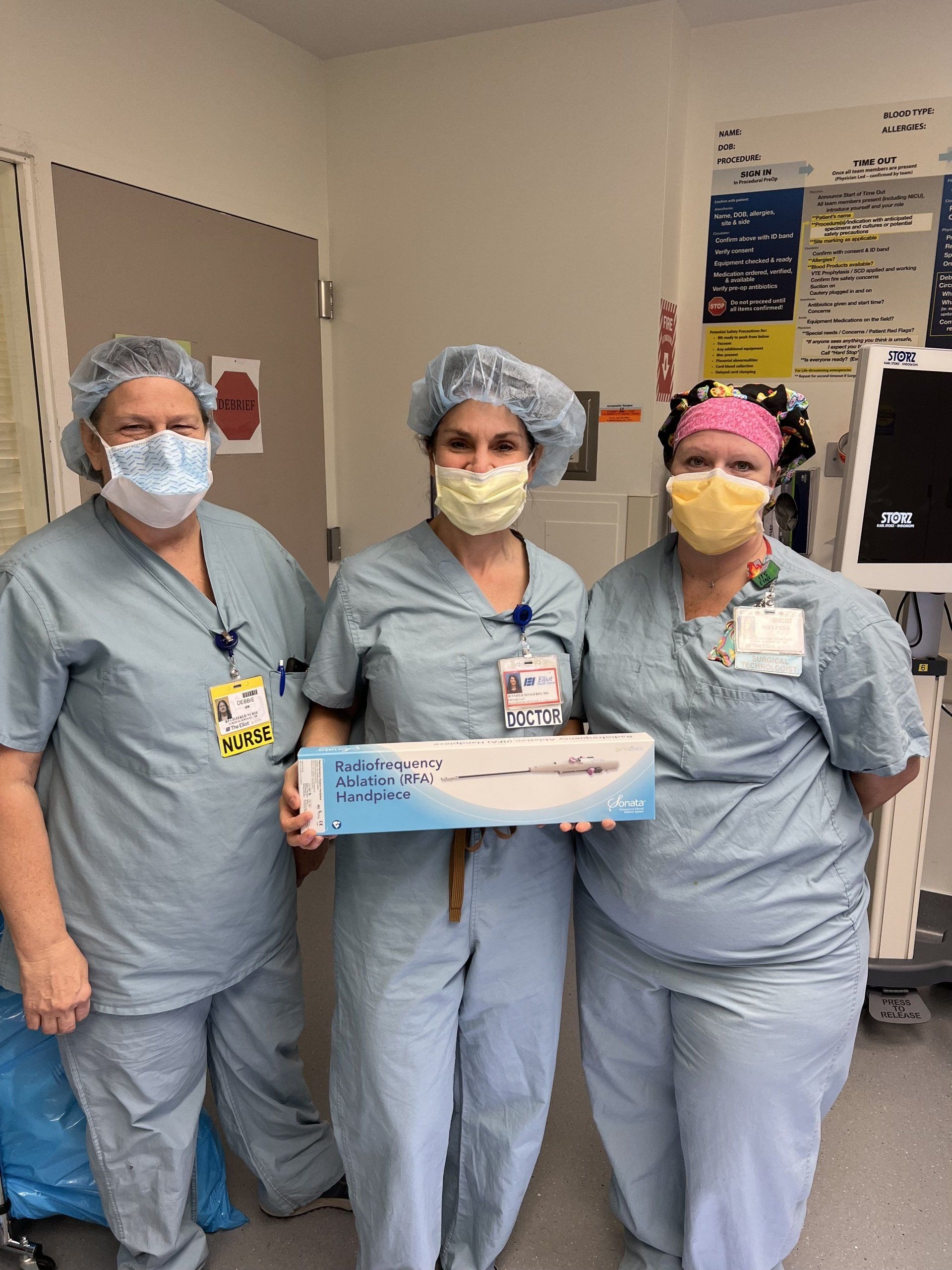
Fibroids, Sonata
Fibroids are benign muscle growths of the uterus. They can be single or multiple and can be found throughout the uterus. Sizes can vary greatly from less than an inch to 10 inches or more. Many fibroids are asymptomatic but they can be associated with heavy menstrual bleeding, spotting, pelvic pressure, pelvic pain, cramping, pain with intercourse, urinary frequency, infertility, and miscarriage.
There are many ways to treat fibroids including myomectomy (removal of the fibroids), hysterectomy (removal of the entire uterus) or Sonata treatment.
Sonata is an incisionless outpatient procedure that treats fibroids from the inside of the uterus. Our office is the first in the state to offer this treatment! Learn more here.
Sonohysterography
Cost-Effective In-Office Procedures
- Avoidance of general anesthesia.
- No fasting.
- Time savings. Your procedure is more likely to run on time if performed in our office. You will also need to spend less time in our office before and after your procedure than you would be required at the hospital or surgery center.
- Cost-efficiency. Your out-of-pocket expense is typically much less in an office setting than a hospital or surgery center.
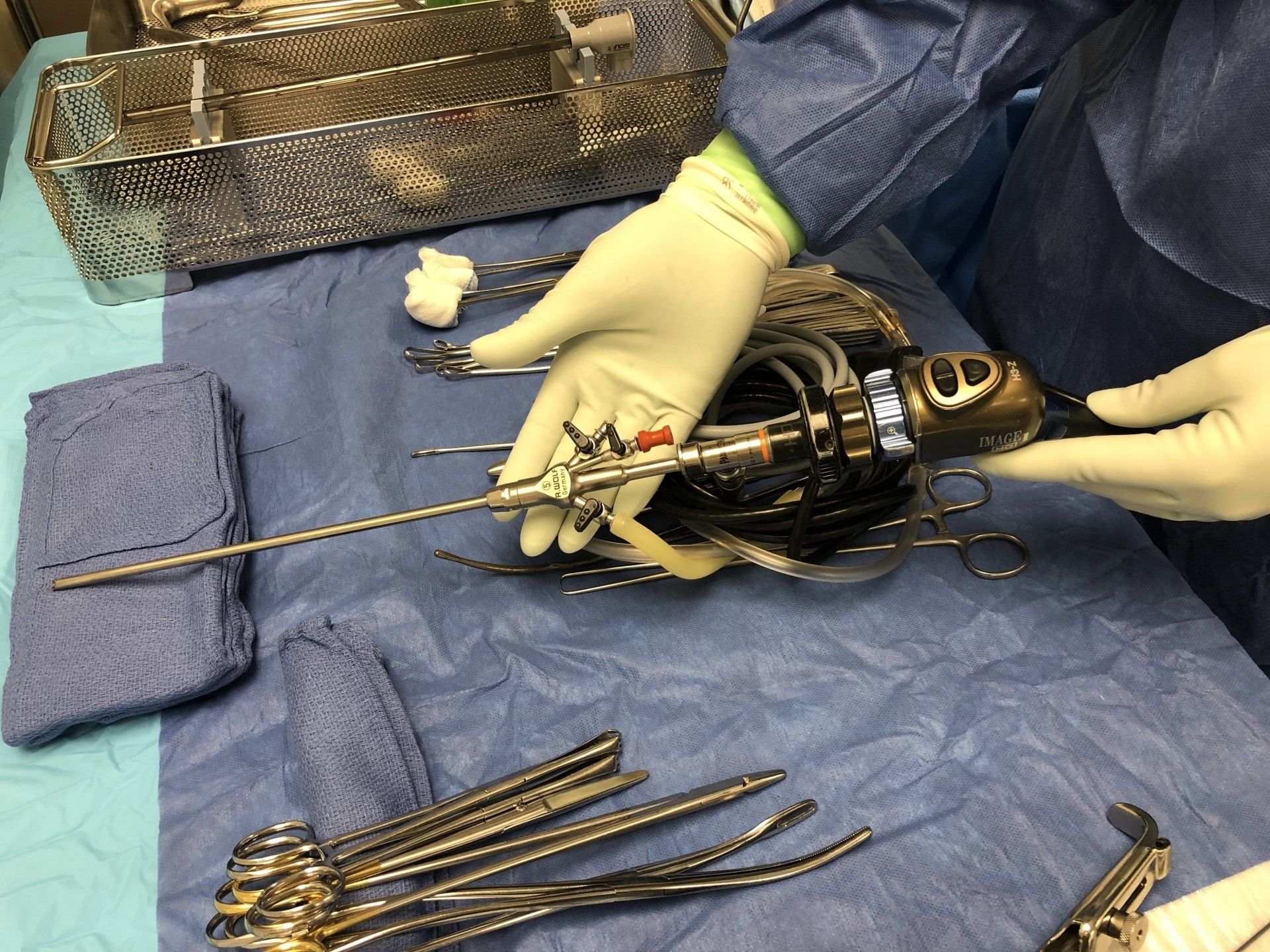
Hysteroscopy, TruClear

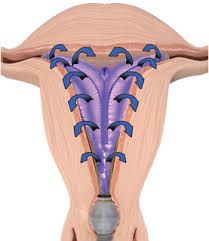
Endometrial Ablation
Hysterectomy
- Vaginal hysterectomy (the uterus is removed through the vagina)
- Laparoscopic hysterectomy/ Laparoscopic-assisted hysterectomy (small incisions with guidance by a camera)
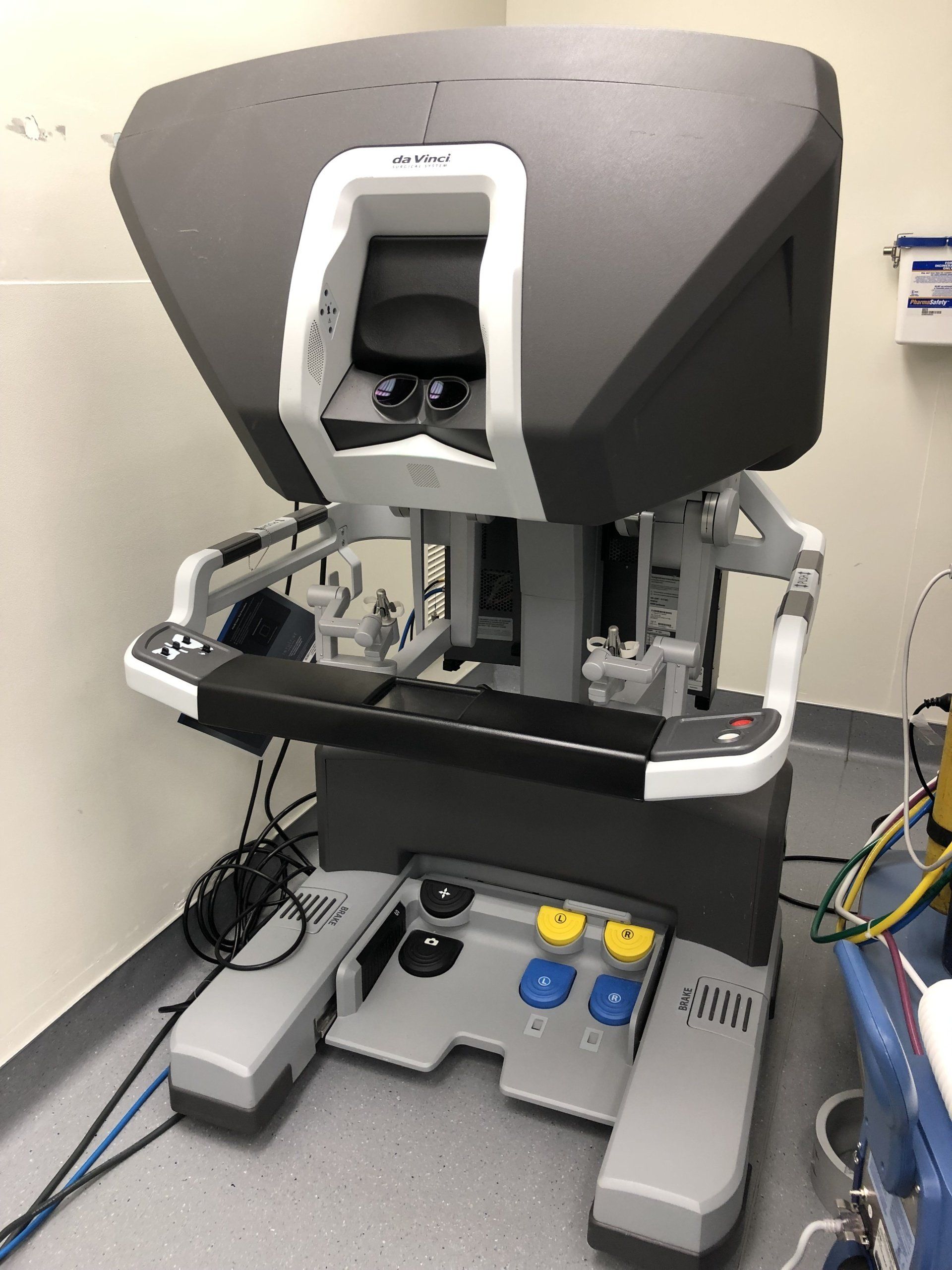
- Robot-Assisted Laparoscopic Hysterectomy (using a Robotic system of surgical tools from outside the body through small incisions that assist to perform the surgery)
Laparoscopy
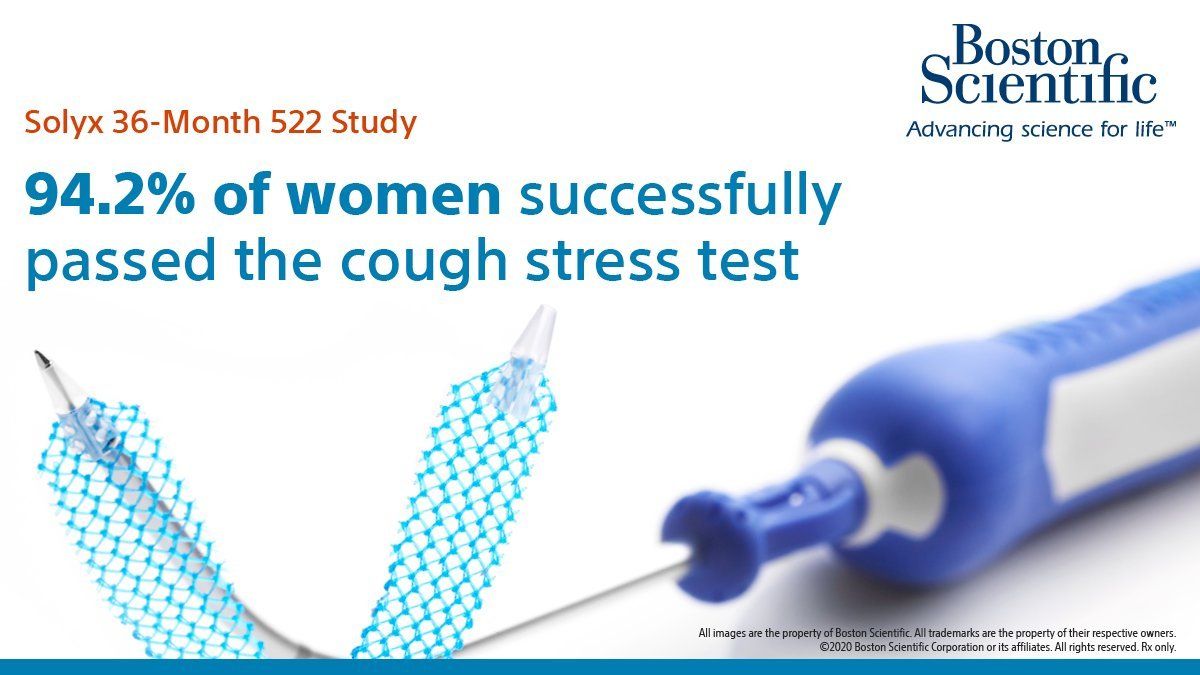
Urinary Incontinence, Urodynamic Testing, Incontinence Treatment and Surgery, Solyx
Learn more about treatment options for incontinence, including the Solyx Single Incision Sling here.