Personalized Obstetrics Services in Manchester, NH
OB Navigation Links
Obstetrical Services We Provide
- Preconception counseling
- Genetic testing
- Certified nuchal translucency ultrasound
- Level II screening ultrasound
- High-risk obstetrical care
- Access to nutritional counseling
- Diabetes screening and education
- Antenatal testing for high-risk pregnancies
- Non-Stress Test
- 3D ultrasound
- Immunizations
- Depression screening
- Postpartum depression support
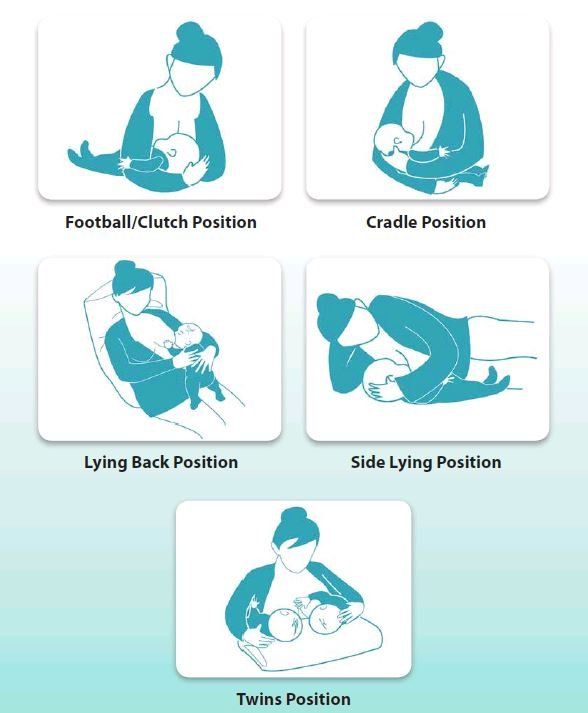
- Lactation consultation
- Delivery at Elliot Hospital, by the doctors you meet in the office, with Level III NICU support
Appointment Schedule
Carrier Screening, Genetic Screening, Genetic Testing
Carrier screening looks for disorders that can be inherited from one or both parents and lead to significant physical impairment or shortened lifespan. A review of your family history helps decide what testing is recommended. These can include Cystic Fibrosis (CF), Spinal Muscular Atrophy (SMA), Fragile X and Tay Sachs.
- CF is a chronic respiratory disease. Caucasians are more commonly carriers of this class of genetic mutation, however, both parents have to pass on the gene for the disease to be present.
- SMA is a severe form of muscular dystrophy that leads to significant physical disability and shortened lifespan.
- Fragile X is most often expressed as varying levels of mental delay in boys and girls. Girls can be silent carriers or can experience gynecological issues later in life.
- Tay Sachs results from an error in metabolism that leads to physical, neurologic and developmental delays and, ultimately, early death.
- Additional testing may be offered based on your ethnicity or family history.
This testing is not mandatory.
Genetic Screening
- We currently offer Non-Invasive Prenatal Testing (NIPT) which screens for Down Syndrome (Trisomy 21), Edward's Syndrome (Trisomy 18) and Patau Syndrome (Trisomy 13). This testing can be done as early as 10-12 weeks and looks for fragments of the baby's genetic material in maternal blood. Since this test is performed on a maternal blood sample there is no risk to the pregnancy. If there is an abnormal result, options for additional testing will be discussed (see Genetic Diagnostic Testing).
- We also offer AFP (alpha-fetoprotein) screening at your 16 week visit. This is another maternal blood draw that looks for neural tube defects like spina bifida.
This testing is not mandatory.
Diagnostic Genetic Testing offers the most complete look at the baby’s chromosomes. With this invasive form of testing, cells are taken either from the fetal parts of the placenta (chorionic villus sampling or CVS) or from the amniotic fluid surrounding the baby (amniocentesis) and all of the baby’s chromosomes are tested. The advantage is more complete testing with 99.9% accuracy. However, there is a small risk of miscarriage.
- CVS is performed in the first trimester (10-12 weeks). Risk of miscarriage is 1/100 (1%).
- Amniocentesis is performed in the second trimester (16 weeks). Risk of miscarriage is 1/300 (0.3%).
Click on the following links for Natera billing information:
Click here for more information:
Frequently Asked Questions
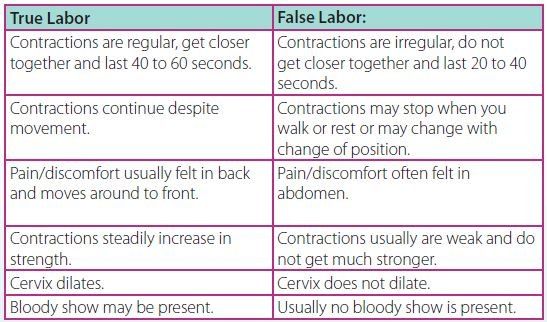
Preparing for Labor and Delivery
Labor and Delivery
Breastfeeding
Postpartum Depression
| POSTPARTUM “BLUES” | DEPRESSION AND ANXIETY DURING PREGNANCY AND POSTPARTUM | POSTPARTUM PSYCHOSIS | |
|---|---|---|---|
| How common is it? | NORMAL. 50-80% of women experience the blues. | 15% - 23% of women, more often in teens. 10% of men. | 1-2 per 1000 women. More often if someone has a history of mental illness. |
| When does it start and how long does it last? | Can occur any time in the first week. Usually gone by 2-3 weeks after birth. | Can occur any time in pregnancy or the first year after birth. It can start gradually or suddenly. Unless treated, it may not go away. | Usually occurs within the first 4 weeks after birth. Needs treatment immediately. |
- Frequent crying
- Sleep disturbances (insomnia/excessive sleeping)
- Appetite disturbances (eating too much or too little)
- Anxiety/panic attacks
- Feelings of anger/irritability
- Over-concern or lack of concern for baby
- Scary thoughts or mental pictures
- Reliving past trauma
- Feelings of guilt and worthlessness
- Feeling overwhelmed/unable to cope
- Loss of interest in things you previously enjoyed
- Fear of harming baby or yourself
- Seeing or hearing things that others do not.
- Agitation, restlessness, irritability
- Mania: feeling speeded up, distracted, excitable, having a decreased need to sleep, or exhibiting fast, pressured speech
- Confusion
- Paranoia (extreme fears)
- Extreme mood swings
- Inability to reason, delusions
- Thoughts or plan of hurting yourself or baby
- Call us at 622-3162 to schedule an appointment. We have nurse practitioners who specialize in perinatal behavioral health and we are known for our compassionate care.
- Treatment may include counseling/therapy or medications that are safe during pregnancy and breastfeeding.
- We recommend good self-care including 4-5 consecutive hours of sleep, small, healthy, frequent meals, exercise, and limiting caffeine.
- There are also pregnancy/postpartum depression support groups so you can connect with other new moms experiencing similar issues.
- Manchester Mobile Crisis Response Team: 1-800-688-3544
- Concord Mobile Crisis Response Team: 1-844-743-5748
- Center for Life Management (emergency services for Derry): (603)434-1577, option 1
- New Hampshire Coalition Against Domestic and Sexual Violence: 1-866-644-3574
- Manchester YWCA Women's Crisis Line: (603)668-2299
- Suicide Prevention Hotline: 1-800-273-TALK (8255)